High Calcium
High-Calcium Consequences
If your serum calcium was elevated on blood testing, that is if your calcium was above 10 mg/dl, the first thing that should be done is to have it repeated. In a large population study done in California a few years ago, in almost 2/3 of the times, a repeat level will be normal. If a repeat level is normal, then another calcium level should be checked. If both re-checks are normal, then nothing else is necessary in many cases, though of course any subsequent testing should be monitored closely. And if any calcium measurement is especially high, like 10.8 mg/dl or higher, then a PTH level should definitely be obtained even with a single calcium result.
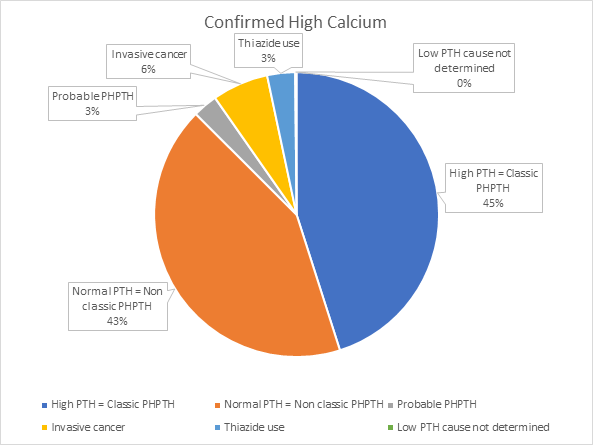
If the serum calcium is high again on repeat testing, then the most likely cause is a benign parathyroid tumor, in fact that is the case about 90% of the time. Although it’s possible for a cancer to be the cause, this is only the case about 6% of the time. For those with a cancer as the cause, in most cases the cancer diagnosis was already known. So if those patients with known cancer are excluded from the group, then a parathyroid problem is the cause in about 97% of cases.
Benign Parathyroid Tumors
These benign parathyroid tumors are more common than many realize, even though most people will never hear of parathyroid glands until they are diagnosed with having a benign parathyroid tumor causing their calcium to be high. Parathyroid tumors are more common in women, and the incidence increases with age. For an entire population, the incidence is estimated to be about 1 out 1300 men and 1 out of 400 women. In elderly women, this increases to 1 out of 200, and for elderly men, 1 out of 400.
In many cases, a person with high calcium may not think of themselves of having any related symptoms. But the associated symptoms are sometimes assumed to be just related to growing older, or related to whatever is going on in a person’s life, such as stress at work or at home, or relationship problems. In other cases, a person knows that something is not right, because of decreased energy levels, fatigue, bone pain, rapid heart rate, sleeplessness, increased urination, thinning hair, or other.
Others may have already had the longer term consequences of a high calcium, such as kidney stones, osteopenia or osteoporosis, atrial fibrillation, or decreased kidney function. There may be cases where there truly are no associated symptoms, but most patients with hyperparathyroidism are significantly affected by it. The good news is that a simple, brief, outpatient operation can quickly cure the problem, with prompt relief of symptoms, and you can learn more about that procedure on this website.
The parathyroid glands are located in the neck behind the thyroid gland. There are four of them, the only gland or organ that we have four of. Basically their only role is to keep the calcium level in a very tight normal range, between about 8 and 10 mg/dl (milligrams per deciliter). You take in calcium in your diet or with supplements, and you store most of it in the bones, but day to day it is essential for your body to maintain this calcium level in the normal range.
The parathyroid glands partner with vitamin D to help absorb calcium from the intestines, and some is excreted daily through the kidneys. If your calcium level trends toward the low side, normal parathyroid glands will increase their hormone production, which will in turn increase the ability to absorb calcium from your intestine, and will also cause your bones to “give back” some calcium into the blood stream. Then when the blood or serum calcium level gets back to normal, the parathyroid glands should decrease their hormone production.
The problem comes when a parathyroid gland starts producing more of its hormone even when the calcium is in the normal range, which then causes the calcium level to continue increasing to abnormally high levels. Why this starts happening in some people is not yet well understood. Clearly there is a defect in the “programming” of the cells, which probably is caused by mutations that develop during the usual cellular replication process, but that’s about as much as is known now. At any rate, this is how primary hyperparathyroidism develops, and the diagnosis is usually very easy to make: if your calcium is too high, then normal parathyroid glands will stop making their hormone (PTH).
If the calcium is high AND the PTH level is high (and it’s very easy to measure), then you definitely have hyperparathyroidism. Even if the PTH level is in the high normal range with a high calcium, that’s still more hormone than is appropriate, so even in this case, the diagnosis is confirmed. If the PTH level is in the lower normal range, it may be necessary to do some more testing to be sure what is the cause. Making the correct diagnosis really depends on comparing the calcium levels to the PTH levels. Sometimes other lab tests will be necessary, like measurement of vitamin D, or albumin.
Schedule a consultation with Dr. John S. Kennedy to learn more about your condition and possible treatments.
“When we catch hyperparathyroidism early, we can cure it before it damages your body. If you have a high calcium level, take it seriously and get tested.” — Dr. John S. Kennedy
Incidence and prevalence of primary hyperparathyroidism in a racially mixed population.
J Clin Endocrinol Metab. 2013 Mar;98(3):1122-9. Yeh MW, et al.